A hundred million Indians are affected by type-2 (non-auto immune) diabetes; one in every five diabetic patients worldwide is an Indian. Knowing the mechanics of diabetes is crucial in designing the best treatment methods. In this, researchers at the Indian Institute of Science, Bengaluru, have tasted success.
First, here is what is already known about diabetes. Cells, known as beta-cells, in the pancreas produce and store insulin, a hormone that keeps glucose levels in blood under check. However, alongside insulin, the beta-cells also produce a protein called ‘islet amyloid polypeptide’, or IAPP.
Sometimes IAPPs aggregate, which ends up killing beta-cells — the consequent dip in insulin production leads to diabetes. In a way, beta-cells end up creating their Frankenstein’s monster.
What prevents this from happening is the body’s defence mechanism known as ‘extracellular vesicles’ (EVs). These are ‘bubbles’ released by cells that transport molecules such as proteins and RNA from one cell to another. The EVs are produced by ‘multivesicular bodies’ (MVB) inside cells. When beta-cells are stressed, the MVBs produce EVs, which prevent the harmful accumulation of amyloid proteins.
IISc research
In their study, researchers at the IISc’s Department of Developmental Biology and Genetics (DBG), led by Nikhil R Gandasi, compared the functions of two secretory vesicles in the insulin-producing beta-cells of the pancreas.
Using a technique called ‘fluorescent tagging’, they showed that MVBs were low in beta-cells of type-2 diabetics, compared with normal individuals. “This showed that loss of insulin secretion in type-2 diabetic beta-cells could also be driven by decrease of MVBs, leading to beta-cells dysfunction, and hence lower number of insulin secretory granules,” says a write-up from IISc.
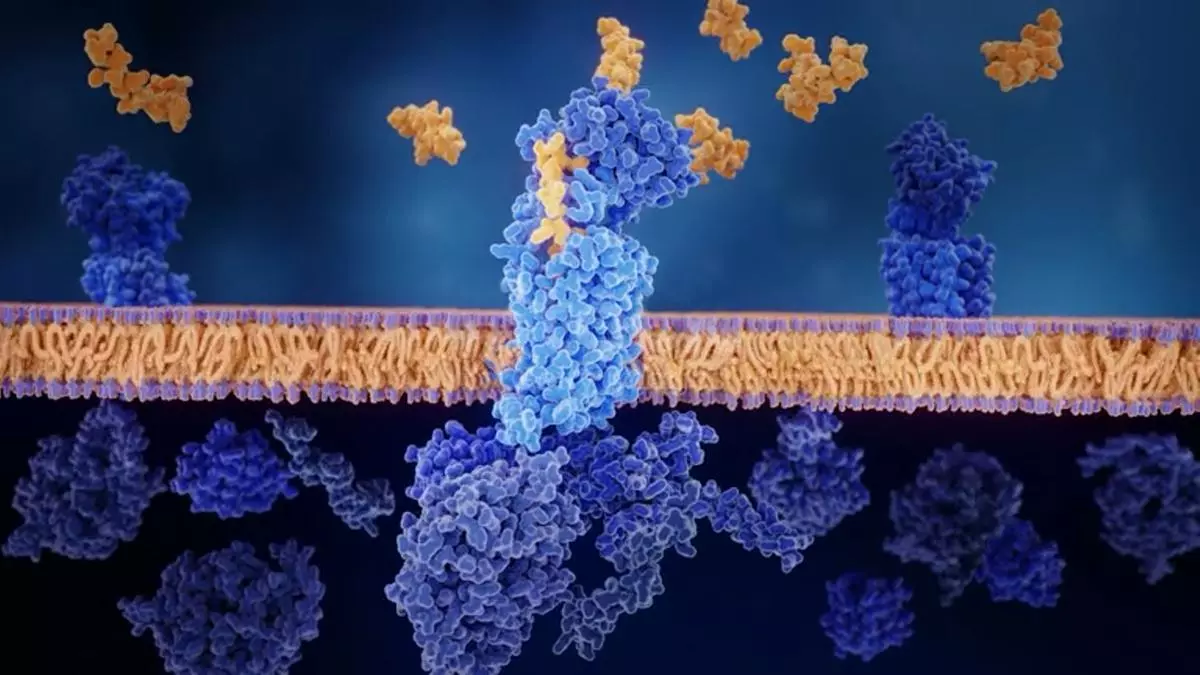
What does this mean in terms of a potential cure? The discovery paves the way for a new method of treatment — using ‘small molecules’ (less than 900 daltons) that can be sent inside cells, past the cell wall (membrane), to interact with, and influence the functioning of proteins, DNA, RNA and other cellular components.
The use of small molecules has been attempted in many other treatments but is relatively new in the context of diabetes. The IISc finding promises just that. Importantly, this would be a drug-free approach to tackling diabetes, by strengthening the body’s natural defence mechanisms.
Now the researchers are focusing on developing small molecules that can do the trick. If successful, it could protect beta-cells by enhancing their ability to clear toxic protein aggregates and step up insulin secretion.
Discovering the right small molecule for this task may not be all that difficult with the assistance of AI, but research must check for unintended effects on other cells, and whether EV production is scalable.